Climate change is a grave concern, and it is our collective responsibility to take action to mitigate it. But, have you ever considered that your inhaler may be contributing to climate change? Inhalers use hydrofluoroalkanes (HFAs), which release greenhouse gases, causing harm to the environment. According to a study by Fraser Health, inhalers generated 8,478 tonnes of carbon dioxide in the Fraser Health region between 2016 and 2021. This is equivalent to about 22% of all emissions from Fraser Health facilities. Moreover, using an inhaler can have a significant carbon footprint; one blue inhaler of Salbutamol has the same carbon footprint as a 139-kilometer car trip. However, the good news is that there are HFA-free alternatives available, which are equally effective for most patients and do not have a negative impact on their health or comfort. Switching to a low-carbon inhaler can reduce the inhaler’s carbon footprint by up to 78% per year and may also improve respiratory care.
Fraser Health is committed to advancing a low-carbon health system and is encouraging discussion around alternatives to metered-dose inhalers containing HFAs. According to a recent survey of Fraser Health residents, 85% agree or strongly agree that it is important for the health system to reduce its carbon footprint and waste. Therefore, switching to a powdered formulation can be an easy step towards reducing your carbon footprint. Not only will you be treating your asthma effectively, but you will also be contributing to the fight against climate change.
Moving on to a more positive note, Monash University is leading the charge in saving the lives of new mothers worldwide. A phase 1 clinical trial has started to test a new, exciting technology – an inhaled powder designed to prevent postpartum hemorrhage (PPH). PPH is a life-threatening complication of childbirth that affects millions of women worldwide, primarily in low- and middle-income countries, and causes excessive bleeding after birth, leading to the deaths of around 70,000 women globally every year. The current treatment method involves injecting the hormone oxytocin into the mother’s vein or muscle during or after birth. However, the new, inhalable oxytocin powder being tested by Monash researchers doesn’t require refrigeration, is non-invasive, easy to use, and most importantly – affordable. By developing an inhalable form of the hormone oxytocin, Monash University is making it easier for new mothers in poorer countries to get the life-saving treatment they need.
Oxytocin works by helping the uterus contract, which prevents excessive bleeding after childbirth. Monash University has developed an inhaler, called the ICOone, for use with their oxytocin powder. The current clinical trial will test the novel treatment on volunteers to assess its performance compared to the current method of administering oxytocin by injection. The researchers hope that the results of the clinical trial will demonstrate the effectiveness of their novel oxytocin delivery system so that it can be delivered to the countries where it’s needed the most.
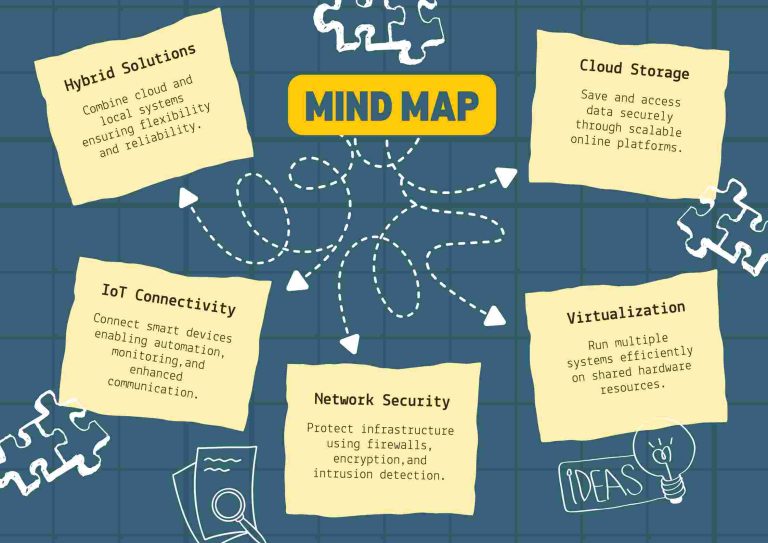
If you have asthma or chronic obstructive pulmonary disease (COPD), you’ll be pleased to know that the latest technology is being used to help you manage your condition. Digital inhalers, which have existed for 30 years, have become more sophisticated, and they now connect patients with accompanying platforms. This change could revolutionize how we manage these chronic illnesses. For example, the Madison, Wisconsin-based digital health company Propeller Health connects patients using digital inhalers with an accompanying platform. Adherium has also developed a digital inhaler system focusing on patient adherence, remote monitoring, and data management.
Despite the challenges of implementing digital inhalers on a larger scale, the potential benefits for patients with asthma and COPD are enormous. Improved medication adherence, better asthma control, and the ability to track inhalation quality and technique could all lead to better health outcomes for patients.
In conclusion, the field of respiratory medicine is undergoing a revolution, with new technologies and innovations that can improve patient outcomes and reduce the impact on the environment. From low-carbon inhalers to inhaled oxytocin for preventing postpartum hemorrhage, these advances hold enormous promise for patients around the world. However, to fully realize their potential, we must continue to invest in research and development, support innovation and adoption, and prioritize the needs of patients. By doing so, we can ensure that everyone, regardless of where they live, has access to the best possible respiratory care.